Syrian experiences of culturally-sensitive mental health and psychosocial support: a Southern African perspective
Mokhantso Sekhesa
JLI Intern

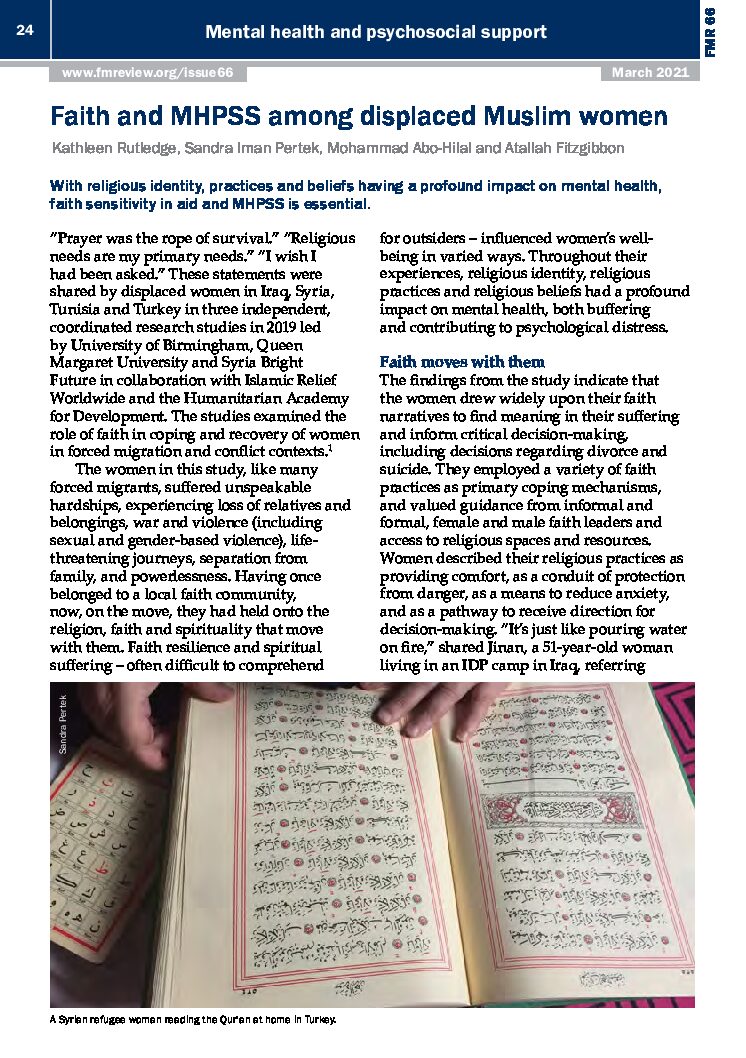
Addressing mental health and psychosocial issues is complex in many contexts. This is the case in Lesotho and South Africa where I live and have lived. In these countries, we ask questions such as, “Could depression that results in negative coping behaviours be related to witchcraft? Is an offering to the ancestors the answer to the self-destructive consequences of addiction?” In the Lesotho and South African contexts, people make meaning and seek healing through faith, beliefs, and culture. This is especially true for most things that are difficult to understand, such as those related to the mind. Integration and awareness of the coexistence, instead of ignorance, of traditional practitioners in modern medical practice is essential. These are the reflections from my countries that I bring to this blog post and my analysis of the Joint Learning Initiative (JLI) – Syria Bright Future (SBF) recent policy paper on mental health and psychosocial support services (MHPSS) in Syria.
The Syrian experience reflected on in this blog highlights a challenging reality in the area of MHPSS. Despite holding such an important place in the lives of most people, faith and the larger umbrella of all cultural beliefs and practices, still have a long way before their full integration into current health practices.
Evidence on MHPSS, culture and faith from Syria
The SBF team, led by Dr Mohammad Abo-Hilal, and supported by JLI, carried out research situated within the local health system in Syria in 2022. They conducted 20 interviews with MHPSS professionals to obtain information about cultural adaptation and faith sensitivity from the providers’ experiences. Involving local stakeholders in the research that is meant for their communities is an effective way to make the research work for the people it aims to serve. Local stakeholders know their contexts best. This places them in a better position to provide insights and help make recommendations more viable and likely to be accepted in those contexts.
The findings from this research highlight the reality of the divide between development-related work and spirituality:
- Providers don’t really understand the concept of cultural adaptation in their services. There is still a lack of clarity about how to practically apply culturally adapted services with a high level of quality in MHPSS.
- Related to the previous issue is lack of training of providers to give culturally sensitive MHPSS.
- MHPSS itself is not considered holistically because the spiritual care aspect in the healing process is left out. This was seen from the difficulty some providers have collaborating with spiritual carers.
- In some instances, there is resistance from MHPSS providers to make adaptations to ‘scientific evidence’. This raises the question of why an approach should be maintained if it doesn’t work. Shouldn’t there at least be adaptations to the context?
Policy/practice recommendations
The authors suggest four main recommendations to address these issues:
- The idea of a paradigm shift, wherein people are supported to engage more critically with faith and culture within the mental health space, is core among the recommendations. Increasing receptivity of the idea that culture and faith have a place in MHPSS might help the willingness to understand cultural adaptation. This, in turn, could reduce resistance to customizing ‘scientific’ approaches to fit the cultural context in which they are applied.
- Another important step is research to raise awareness and uptake of cultural adaptation practices in MHPSS for the Syrian context. Strengthening the evidence base can help to create a convincing case for holistic healthcare and the importance of including spiritual care practitioners in providing holistic MHPSS.
- With the correct mindset and evidence, appropriate training and curriculum development can fill knowledge gaps and improve collaboration among local professionals, researchers, and spiritual caretakers in MHPSS. This also speaks to the final recommendation.
- The final recommendation to address issues in MHPSS is partnership, coordination, and awareness-raising among various stakeholders, using a variety of means of communication.
Final thoughts
Understanding communities’ perspectives and beliefs is critical because those viewpoints are reality for those who hold them. Faith and culture cannot be separated from mental health services if the latter are to be fully responsive to people’s needs. To separate the two is to render mental health services ineffectual for many people. In my experience of Lesotho and South Africa, people still very much connect to their indigenous culture for various needs, including mental health issues. At the same time, the introduction of different medical and social practices, including science, has meant most populations have adjusted to include ‘scientific’ medical methods to deal with health issues they don’t understand. The challenge arises where it is difficult to integrate science and culture. People still hold their cultural beliefs, but there seems to be an underlying message that in MHPSS, one cannot adopt both cultural and scientific practices. Therefore, the recommendation of a paradigm shift using research, among both MHPSS practitioners and the population, is critical in integrating science and culture to more effectively address mental health issues.
Understanding the Syrian experiences of culturally-sensitive mental health and psychosocial support is crucial. In the Southern African context, shared narratives enhance our global perspective on resilience and healing. Integrating cultural nuances in interventions fosters empathy and inclusivity. Embracing diversity is a collective responsibility. #tg macro #GlobalMentalHealth